Corona Virus (SARS-COV2) UPDATE
March 28, 2020
Corona Virus (SARS-COV2) UPDATE
Padmini Arhant
Coronavirus Cases: 663,740
Deaths: 30,879
Comparison between the original epicenter Wuhan, Hubei Province, China and the current leading Victim nation USA:
Total Cases as of date – Saturday, March 28th, 2020.
USA – 123,750. China – 81,439
New Cases:
USA – +172. China – +45
Total Deaths: –
USA – 2,227 China – 3,300
New Deaths:
USA – +6. China – +5
Total Recovered:
USA – 3,231. China – 75,448 (?) – this is a vast contrast.
Active Cases:
USA – 118,292 China – 2,691 (?) – this again do not match the ground reality.
Serious Critical:
USA – 2,666. China – 742
Total Cases /1M pop:
USA – 374. China – 57 (?)
Deaths /1M pop:
USA – 7 China – 2
USA 1st Case – January 20th, 2020
China 1st Case – January 10th, 2020
Further update on the drug research and other details related to corona virus SARS-CoV2 virus.
Please find below samples of articles and explanations from medical community on the corona virus SARS C0V2. Please refer to the original links for the content source. Thank you.
1. Reference: weforum.org – World Economic Forum on Corona Virus SARS CoV2
https://www.weforum.org/agenda/2020/03/covid-19-explained-virology-expert/
Belgian virologist Guido Vanham, the former head of virology at the Institute for Tropical Medicine in Antwerp, Belgium, helps answer questions about COVID-19’s origins, its behaviour and its future.
Many people still compare this virus to SARS and believe the measures taken by governments are excessive. Why should we not compare it with SARS? Is it more dangerous?
We have to compare it with SARS because it looks very much like SARS. The relationship between this virus and SARS is very close: they have many identical parts in their genome, so it is really to some extent a SARS-2 virus. It is, however, much more infectious. The estimation now is that any person infected with this virus may infect three other people, which leads to an exponential growth of the epidemic – that was not the case with SARS. It is also clear that people without symptoms can spread the virus.
Can we explain why it is so infectious?
No. There is some understanding of why SARS, MERS and COVID-19 are related and why they produce heavy symptoms, but why this particular virus is much more infectious than other related viruses is something we still do not know. That is a matter of research. Remarkably, the previous SARS Cov1 and the present SARS CoV2 use the same “receptor” for entry in cells and the suggestion is that the “envelope proteins” of the present SARS CoV2 are just more efficient in using the “entry door” into the lung cells and elsewhere in the body.
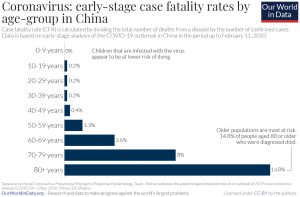
How have fatalities from COVID-19 in China varied by age group?
Image: Our World in Data
2. Reference: https://www.davidson.edu/news/2020/03/05/davidson-expert-what-we-know-about-new-coronavirus-strain – Thank you.
Dave Wessner, biology professor and interim chair of health and human values, studied the pathogenesis of coronaviruses as a post-doctoral researcher at the Uniformed Services University of the Health Sciences.
Now, Professor Wessner on the appearance of SARS-CoV-2
We caught up with Wessner to learn more about the coronavirus.
What do we know about this strain of the coronavirus?
Coronaviruses are not new; we’ve studied them since the 1960s. In fact, certain coronaviruses are among the pathogens that cause the common cold. However, the strain behind COVID-19 is new.
How does a virus like SARS-CoV-2 suddenly appear?
A lot of this is still unclear. We just haven’t had enough time to study the origins of this virus, but apparently this virus jumped into the human population from a wild animal. I’ve heard speculation that it came from bats or from civets.
How does it leap from one species to another?
Viruses are known as very messy microbes. They replicate very quickly and mutate very rapidly. To complicate matters, a coronavirus is an RNA virus—rather than having a double-stranded DNA genome like we do, it has a single-stranded RNA genome which makes it more error-prone than a DNA virus.
If a mutant appears that is well adapted to the non-natural host, it’s going to thrive. And when viruses switch species, they are frequently much more virulent than they are in the natural host.
Is this kind of leap from one species to another unusual?
No, this happens all the time. HIV is a good example of this kind of transition. HIV started as a simian virus that got transmitted from a chimp to a human and mutated to adapt to humans.
In fact, transfers from non-humans to humans are occurring more often because we’re expanding more. If there’s a virus affecting mammals deep in the Amazon, there are more chances for it to spread because there are increasing interactions between humans and non-humans.
Fortunately, most often, these are dead-end transmissions. We see that periodically with influenza. H7N9, a virus that presumably moved from chickens or ducks, has been lethal but the spread has been very limited.
How do you gauge the threat a virus might pose?
There are two things to consider: How easily is the virus transmitted, and how fatal is it?
The ebola virus, for example, is highly lethal, but it is not rapidly transmitted because it is spread through bodily fluids.
Meanwhile, measles, which we have largely eliminated due to widespread vaccinations, is less lethal, but highly contagious because it is spread through coughing and sneezing.
The COVID-19 virus appears to be respiratory, which likely means it spreads quickly. It’s too soon to tell how lethal it is—the current estimate of two percent lethality could change a lot. But even if it has a very low lethality rate, if millions are infected, that still means a lot of deaths.
How might researchers be studying the virus right now?
One of the first steps is to figure out where it came from so you can see how much it has mutated. That means you isolate the virus from humans and from the wild animals and sequence the RNA of both viruses. Then, you compare the sequences to see how similar they are. That information will help researchers to begin developing possible treatments or vaccines.
When I studied coronaviruses, we were working to understand the interaction between the virus and the host cell. Viruses can only replicate inside the host cell so they have to pass through the outer surface of the cell via a specific protein receptor. We were trying to identify that protein because if you could figure out which protein gave it access to the cell, you could work to block that interaction.
—————————————————————————————————–
3. Research on Drug and Vaccine to contain SARS – COV2 or Corona Virus.
Segment from Original Source 60 Minutes Australia https://youtu.be/NeY_HqIasdo – Thank you.
Written by Padmini Arhant · Filed Under Featured, Health | Leave a Comment
 PadminiArhant.com
PadminiArhant.com